Can migraines be prevented?
While headache is a common pain that can usually be treated with a few pills, migraine is a neurological condition that affects 10% of the population and can make life almost unbearable at times. Research by the Sperlágh group could pave the way to help prevent and treat this serious condition.
While headache is a common pain that can usually be treated with a few pills, migraine is a neurological condition that affects 10% of the population and can make life almost unbearable at times. Research by the Sperlágh group could pave the way to help prevent and treat this serious condition.
Migraines are one of those diseases that people talk about openly, not just empathize with their sufferers. Although there are several theories about the causes of migraine, there are unfortunately no theories to prevent it from developing, and in many cases, the treatment is not effective enough. Today's fast-paced, often irregular lifestyle, compounded by sleeplessness, overwork, inadequate diet, and all kinds of self-induced stress (light, sound), certainly contributes to the increasing number of people suffering from it, but it is not a disease of our time. It was known and even treated in ancient Egypt. Although Egyptian pharmacists prepared their medicines according to precise recipes, and many of them could still be used today, their treatment for migraine is unfortunately not one of them. One could even make a clay crocodile and put the herbs listed on the ancient papyrus in its mouth, but it is unlikely that tying it to the patient's head would make the migraine go away.
As migraines are not a fussy disease, many famous people have suffered and continue to suffer from them. One of them should be known to every Hungarian schoolchild from the novel The Sons of the Man with a Heart of Stone by Jókai. He is Haynau, the "executioner of Brescia", a fearsome figure of the reprisals after the 1848-49 war of independence, who is visited by the vengeful Plankenhorst Alphonsine during a migraine attack. But the headachy Haynau turns against those who are trying to revoke his assignment and unexpectedly shows mercy to all. Of course, we also learn from Jokai that Haynau's headache attacks were caused by a head injury, which is certainly true since among the many causes of migraines is a head injury, which Haynau has suffered on several occasions.
But now, after ancient papyri and 19th-century history, let those who have chosen migraine as one of their research topics speak out.
Academician Beáta Sperlágh's Molecular Pharmacology group investigates the role of purinergic signaling in the physiological and pathological functioning of the nervous system. Their article, published in the British Journal of Pharmacology, the most prestigious journal of pharmacological research, with Fóra Gölöncsér as the first author, is on this very disease that causes so much pain.
- It is clear that both migraine and headache are manifestations of abnormal functioning of the nervous system, but what is the main reason why neither the prevention of headache nor the truly effective treatment of migraine is yet solved?
Flóra Gölöncsér :
- We are talking about a complex disease, the pathogenesis of which is not fully understood. Currently, there is no biomarker for the diagnosis of migraine. Gender, genetic, hormonal, and metabolic factors play a role in its development, as well as external environmental and pharmaceutical factors.

Beáta Sperlágh :
- Although we have some drugs that can relieve migraine attacks, such as serotonin agonist triptans or antagonists against CGRP, a peptide (protein) released in the brain and causing inflammation in the meninges, these drugs do not work in all migraine patients, and the optimal solution would be to prevent migraine attacks. Unfortunately, such an agent is not yet available. The main reason for this, as Flora mentioned, is that migraine is a complex condition caused by a combination of pathological hypersensitivity of the nerves that innervate the meninges and vascular factors, and is therefore very difficult to control selectively. Furthermore, as in epilepsy, the cause of the seizure, or "trigger", is not well understood yet.
- What can we know about its possible genetic background?
F:
- The fact that the development of migraine is significantly influenced by the genetic background of the individual has been confirmed by family and twin studies. These suggest that migraine is an inherited trait, with a chance of inheritance of between 30 and 60%.
B:
- Genetic mutations are already known to be responsible for the familial form of migraine. However, these affect only a small proportion of migraine sufferers.
- It is known and true that migraine is more common in women. Why is this?
F:
- Migraines are three times more common in women than in men. There is a lot of data on how hormonal changes affect the onset, severity, and duration of headaches. The frequency of migraine onset increases during female sexual maturation, peaking in the late 30s and decreasing rapidly after menopause. The decrease in estrogen levels is thought to lead to increased migraine attacks during menstruation and menopause.
- Is there any evidence that this varies between different ethnic groups or races?
F:
- There are no recent comprehensive data on ethnic groups of people with migraine. A study from two decades ago showed that whites were twice as likely as Asians, blacks, and other ethnic groups to have migraines. This data should be treated with caution, however, as the result may have been influenced by the fact that there may have been considerable variation in the number of visits to doctors, for example, between different ethnic groups, and it may not always have been possible to make an accurate diagnosis.
- In terms of their proportion, are there more migraine sufferers today than in the past and, if so, how much can changing lifestyles be responsible for this?
F:
- It is important to note that the most common headache is not a migraine, but a tension-type headache. In Hungary, there are 1-1.2 million migraine sufferers, which is still a very high number, as it is more than 10% of the population! Nowadays, people do not pay enough attention to getting enough sleep, eating healthy food, drinking enough fluids, and exercising frequently. But if we can make healthy lifestyle changes, the frequency and severity of headaches will decrease. The severity, duration, and frequency of headaches are strongly influenced by the emotional state of the individual, their temperament, stress tolerance, whether they are irritable, and of course anxiety and depression are major risk factors.
- In your experiments, as is common in pharmacological research, you used an animal model. In this work, you induced migraine in mice by nitroglycerin treatment. What made the model setters think that nitroglycerin could do this?
B:
- The use of nitroglycerin (NTG) as a migraine model is based on observation. In acute coronary artery occlusion, commonly known as anginal attack, characterized by acute chest pain, it is almost a matter of course that a severe headache is a side effect after taking the drug. This is so typical that if this symptom does not occur, it is an indication that the expiry date of nitroglycerin has passed.
F:
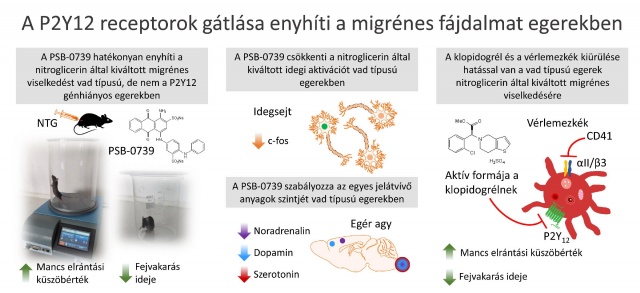
- It has also been observed that systemic administration of NTG in migraine sufferers causes so-called migraine attacks without visual, speech, or movement disturbances (aura). NTG was first used by Iversen and colleagues (1989) in a human model of migraine, while Bates and colleagues (2010) were the first to use NTG in a mouse model, demonstrating that NTG activates and sensitizes the facial innervation (trigeminal) system.
- In human experiments, you can know if a person is having a migraine attack, but how do you know if a poor mouse has a headache? What evidence is there that the effect of NTG in mice is similar to human migraine symptoms?
B:
- The migraine disease that affects humans in mice is not known. As is true in many other cases, the animal model here cannot be identified with the human disease.
However, indirect evidence suggests, that mice experience similar symptoms to humans following NTG administration.
They also exhibit light avoidance, increased head-scratching in response to pain, facial grimacing, and increased sensitivity to pain in other parts of the body, such as the hind limbs. These are also well measured in experiments.
F:
- There is no animal model of migraine that fits all aspects of the disease, so further research is needed. To the similar symptoms listed above, I would also add that similar sensory disturbances have been observed in rodents when exposed to NTG as in humans with migraine. These include increased skin sensitivity to heat, which in mice can be demonstrated by the so-called "hot plate" test following NTG treatment.
- So there is an accepted mouse model of migraine. But how did ATP, the energy source of living organisms as everyone learned in high school, come to be associated with migraine? And what explains the prominent role of P2Y12, a special protein that recognizes and binds ATP?
B.
- The role of ATP in migraine was first suggested by Geoff Burnstock decades ago but the involvement of specific receptor subtypes was not known at the time. Burnstock associated purinergic signaling - the ATP purine base compound - primarily with the vascular theory of the disease.
F:
- There is now increasing attention to the regulation of pain and nerve dysfunction via ATP and ADP-activated P2X and P2Y receptors on facial innervated nerves. These P2 receptors are well known to play a role in the development of pain sensation. The presence of these receptors has also been demonstrated in cell bodies of facial nerve fibres affected by migraine.
- How did you find the P2Y12 receptor in particular when looking for the cause of migraine?
F:
- The presence of the P2Y12 receptor has been detected in several tissues. It is found on vascular smooth muscle cells, but also on microglial cells in the central nervous system. Microglial cells interact with nerve cells to mediate the central nervous system's response to painful stimuli and inflammation. P2Y12 receptors located in the platelet membrane can trigger platelet aggregation following their activation, i.e. when they bind ATP.
Our recent work has demonstrated, that P2Y12 receptor inhibition can prevent the development of migraine-like pain in mice, and that P2Y12 receptors expressed on platelets contribute to this.
- This is a very nice result in itself, but when will it become a drug?
B:
- What makes this result particularly significant is that drugs that inhibit the P2Y12 receptor are widely used in the clinic to prevent stroke and heart attacks!
Consistent with our studies, clinical trials have shown that migraine patients taking the P2Y12 receptor inhibitor clopidogrel, which is also used in our trials for other reasons, the incidence of stroke is also lower.
A three-month study found that clopidogrel reduced the incidence of migraine attacks, and no relapse effect was observed after discontinuation.
Our basic research results are therefore directly applicable to the clinic
- It can be many years before a discovery becomes a drug and reaches patients. What can we expect in this case?
B:
- The launch could happen within a few years because in this case, there is no need for the otherwise lengthy drug development and preclinical trials because we already know that these drugs are safe.
However, we need to prove that preventive treatment is effective by larger clinical trials.
F:
- The P2Y12 receptor is a new potential target for migraine therapy. It is true that in many cases, no drug works to prevent migraine attacks, but our research offers a new option for people with migraine who have not had adequate migraine therapy.
- Research is almost never over. What is the next question?
- In the future, we aim to explore molecular signaling pathways and understand the exact mechanism of action of P2Y12 receptor inhibition.